“We need to stay on the cutting edge of technology. Molecular is the future now and will continue to be the future.”
Prof. James Snyder, PhD
Professor of Pathology and Laboratory Medicine, Director of Microbiology and Infectious Disease Molecular Diagnostics, University of Louisville Hospital
Watch clinician testimonials
Molecular Diagnostics for Hospital treated infections – When Cultures Fall Short

Hospital-acquired pneumonia, infective endocarditis and CNS infections are among the most severe manifestations of healthcare-associated infections (HAIs). Across Europe, HAIs collectively cause ≈ 37 000 deaths and €7 billion in direct costs each year¹. Endocarditis alone kills 13–25 % of patients during hospitalization and another 9–20 % within a year²,³. Yet cultures from bronchoalveolar lavage, pleural fluid, bronchial wash and CSF frequently remain negative especially after prior antimicrobial therapy driving prolonged empirical treatment, higher costs, longer stays and greater clinical risk⁴.
Our Solution:
MicroGenDX tests use next-generation sequencing (NGS) to enhance diagnosis and clinical management of respiratory and systemic infections—especially when cultures fail. Validated sample types include BAL, respiratory swabs, sputum, ETA, and pleural fluid (RespiKEY); whole blood (BloodKEY); and intra-/postoperative swabs, tissue, and fluid (SurgeryKEY). These tests support the diagnosis of:
- Hospital-acquired pneumonia (HAP)
- Infective endocarditis
- Central nervous system (CNS) infections
- Sepsis and bloodstream infections
- Post-surgical infections and more
Combining NGS with qPCR, MicroGenDX enables highly sensitive detection of bacterial and fungal pathogens, even in culture-negative or post-antibiotic cases. Resistance gene profiling supports earlier, targeted antimicrobial therapy—improving diagnostic speed, reducing empirical treatment, and lowering risks of complications, hospital stays, and resistance.
- 1. European Centre for Disease Prevention and Control (ECDC). Estimating the burden of healthcare‑associated infections in Europe. 2008.
- 2. Habib G et al. 2015 ESC Guidelines for the management of infective endocarditis. Eur Heart J. 2015
- 3. Cahill TJ, Prendergast BD. Infective endocarditis. Lancet. 2016
- 4. Binnicker MJ et al. 2024 IDSA‑ASM Guide to Utilization of the Microbiology Laboratory. Clin Infect Dis. 2024
Clinical Insights from our Samples
Extensive Real-World Experience:
By 2025, MicroGenDX had analyzed over 750,000 samples, identifying thousands of distinct microbial species.
Detection Beyond Common Pathogens:
Findings included both common pathogens and fastidious or anaerobic bacteria often missed by culture (e.g., Tropheryma whipplei, Leptotrichia buccalis, and more).
Antibiotic Resistance Gene detection:
Each sample is screened for 17 key resistance genes, enabling targeted antimicrobial strategies and reducing reliance on broad-spectrum empiric treatment.
Proven Clinical Value:
These findings highlight the diagnostic precision and clinical relevance of MicroGenDX’s NGS-based urine testing in urology.
Recommended use of molecular diagnostics and NGS in culture negative samples
IDSA-ASM 2024 Lab Guide – NGS Highlights
Respiratory infections
Both NGS and multiplex PCR are now essential tools in diagnosing respiratory infections. The 2024 IDSA–ASM lab guide recommends NGS for high-risk, culture-negative cases such as severe pneumonia, immunocompromised patients, or unexplained outbreaks. NGS performs well on small volumes of BAL, endotracheal aspirate, or lung tissue, even after antibiotics, and detects fastidious or polymicrobial pathogens often missed by culture.
Other systemic infections (bloodstream, CNS, bone & joint, endocarditis)
For culture-negative but high-risk infections such as endocarditis, prosthetic joint or graft infections, CNS infections, or sepsis NGS is increasingly recommended. The 2024 guide supports its use in low-volume specimens like CSF or ocular fluid and in patients already on antibiotics. Evidence shows NGS outperforms culture in synovial fluid, heart valves, plasma, and CSF, detecting pathogens that guide treatment changes. In these complex cases, NGS often provides the actionable diagnosis when other methods fail.
Miller JM, Binnicker MJ, Campbell S, et al. Guide to Utilization of the Microbiology Laboratory for Diagnosis of Infectious Diseases: 2024 Update. Clinical Infectious Diseases. 2024
“NGS has been a major breakthrough in microbiological diagnostics in the last few years, enabling increased yields in the detection of pathogens.”
“NGS demonstrates a positive clinical impact as a diagnostic tool and its implementation in routine clinical practice has been justified for hospitalized patients with suspected infections…”
“NGS exhibits a distinct advantage over PCR in its ability to detect all bacterial or fungal genetic material…”
- Henríquez L, Uribarri A, Portillo ME. Revisiting diagnostics: practical application of next-generation sequencing technologies for infectious diseases. Clin Microbiol Infect. 2025
Interpreting our lab report
Each test includes a detailed laboratory report, providing clinicians with clear, structured data for fast decision-making.
These reports include:
• List of bacteria and fungi detected in the sample(s)
• Identified antibiotic resistance genes
• Antimicrobials to consideration for treatment
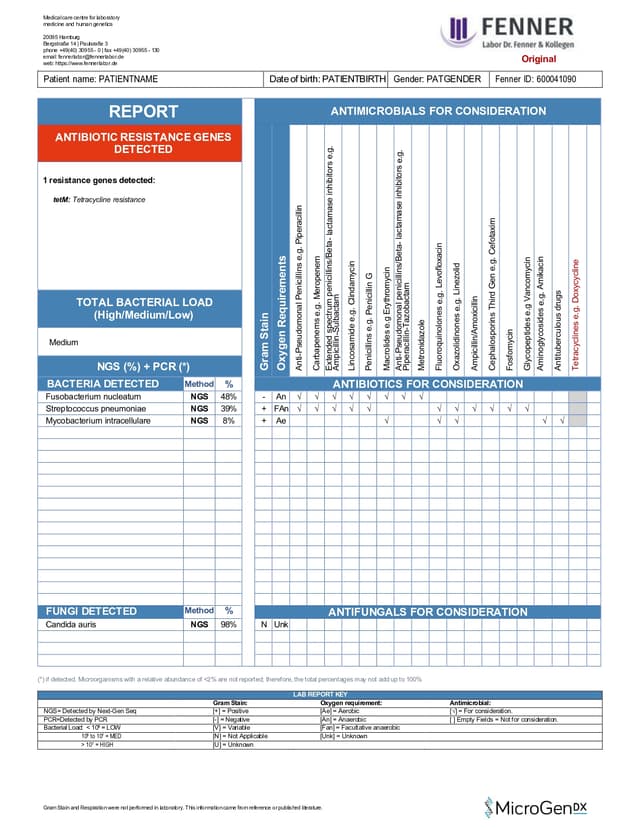


RespiKEY-Test
Lower Respiratory Tract Infection Test
Sputum, Swab, Fluid (BAL, ETA, Pleural fluid)
NGS DNA + qPCR Diagnostics for accurate microbial identification
17 antibiotic resistance genes & list of antimicrobials for consideration
3-5 Business days (excludes transit)


BloodKEY-Test
Blood Infection Test
Blood
NGS DNA + qPCR Diagnostics for accurate microbial identification
17 antibiotic resistance genes & list of antimicrobials for consideration
3-5 Business days (excludes transit)


CSFKEY (MDXCSF)
Cerebrospinal Fluid Infection Test
Cerebrospinal Fluid (CSF)
NGS DNA + qPCR Diagnostics for accurate microbial identification
17 antibiotic resistance genes & list of antimicrobials for consideration
3-5 Business days (excludes transit)
Publications Demonstrating the impact of NGS in Hospital treated infections
Next-Generation DNA Sequencing Enhances Pathogen Detection and Culture negative hospital samples
Study design - Single-centre, retrospective , 105 culture-negative specimens collected in Milan. Different hospital department’s culture-negative samples (48 % orthopaedics, 15 % neurosurgery, 12 % cardiac surgery, others). Each sample was re-analysed with 16S NGS sequencing.
What the study found - Among culture-negative samples, 74.3% (78/105) tested positive to one or more microorganisms through NGS. Single pathogen was detected in 68.6% cases, while two or more pathogens were detected in 5.7% of samples. 31 different strains were detected including: Acinetobacter lwoffii, Facklamia languida, Peptostreptococcus spp., Pantoea cypripedii, Actinomyces spp., Pseudomonas spp., Bacillus vietnamensis, Terribacillus spp.
Why it helps hospitals - Recovering hidden infections enables targeted therapy, uncovers polymicrobial or anaerobic condition early and curbs broad-spectrum antibiotic use and costs.

Heart valve infections
Single-center diagnostic-accuracy study of 51 consecutive valve-surgery patients: 44 met “definite/possible” IE Duke criteria; valve tissue from every case was split for untargeted mNGS and conventional work-up (blood culture, valve culture, Gram stain). About 80 % had received antibiotics pre-op.
mNGS identified a causative organism in 97.6 % of definite IE valves vastly outscoring blood culture (46.2 %), valve culture (17.1 %) and Gram stain (51.4 %). It uncovered fastidious pathogens such as Coxiella burnetii and Bartonella quintana and delivered answers in ~48 h (vs 3–7 d for enriched cultures), supporting mNGS as a rapid, high-yield fallback when cultures fail or organisms are atypical.

Lung infections – BAL samples
Single-centre, retrospective cohort of 81 immunosuppressed adults with connective-tissue disease undergoing broncho-alveolar lavage (BAL) for suspected pneumonia; 62 cases were adjudicated as true infections and their BAL fluid was analysed by mNGS alongside routine culture/PCR/serology.
Results — mNGS detected pathogens in 50/62 infections (81 %), beating conventional microbiology (41/62 = 66 %) and BAL culture alone (21/62 = 34 %). It uniquely flagged opportunistic organisms such as Pneumocystis jirovecii and non-tuberculous mycobacteria, uncovered mixed infections in ~25 % of positives, and drove therapy changes in 18 % of the entire cohort, supporting BAL-mNGS as the favoured first-line test when immunosuppression limits classical yields.

Clinical cases where MicroGenDX test helped achieve treatment success
Fungal infection in mastoid cavity
A 61-year-old male had been diagnosed with severe pneumonia and treated with empiric broad-spectrum antibacterial and antifungal drugs before bronchoscopy was performed. The patient responded poorly to those empiric treatments. Three fungi were found by NGS in the BALF: Pneumocystis jirovecii, Aspergillus fumigatus, and Rhizopus oryzae. Patient clinical improvement was achieved after adjusting to appropriate therapy based on NGS results.
Inquire about our test
Send us a message using the form below, or email us at info@microgendx.eu
